A Holiday Ultrasound “Parfait” Recipe That’s Sure To Be a Hit
Amir Khiabani, MS4, Alabama College of Osteopathic Medicine
Devon Khiabani, MS4, Alabama College of Osteopathic Medicine
Wesley Priddy, MD, USF MCOM — Emergency Medicine Residency
Charlotte Derr, MD, RDMS, FACEP University of South Florida — Emergency Medicine
Background
A little bit of a background on the subject before we dive into the recipe…
An estimated 1 million patients with knee injuries present to the Emergency Department, which represents about 2.5% of the patients seen in ED’s. This goes to show that ED physicians really “kneed” to have a good understanding of these types of injuries (see what we did there). Knee injuries can have many characteristics to their presentation. They swell, bruise, and when there is an intraarticular fracture associated with it, blood and fat can introduce themselves into the joint. Voila! The ingredients to a lipohemarthrosis (LH) parfait!
This parfait gets created by the release of marrow fat into a joint secondary to an intraarticular fracture of a marrow containing bone. Traditionally, the initial evaluation of a knee injury in the ED consists of a plain radiograph, which can visualize a fat-fluid level. However, seeing the parfait sign on x-ray has a relatively low sensitivity for detecting an intraarticular fracture. CT, MRI and US can also aid in the visualization of LH as either a double fluid-fluid level (fat and blood) or a three-layered effusion in the joint (fat, serum and red blood cells).
Yes, you may see a LH on x-ray as well as CT or MRI as the double fluid level/parfait sign, but we at USF Emergency Medicine are ultrasound geeks and thus the imaging modality discussed to diagnose this type of fracture today will be ultrasound. Another point to add to ultrasound is that in some traumatic knee injuries, CT or MRI may not be the best initial option to diagnose intraarticular fractures.
Ultimately, visualization of fluid levels on sonographic imaging is a very specific and reliable indicator that there is likely an intraarticular fracture. The Parfait Sign!
So! Let’s show you how to put these ingredients together using your handy POCUS in the following case.
Case
A 55-year-old female presented to the emergency department due to right knee pain. The patient stated that she fell approximately 1 week prior to arrival and had been to several hospitals since the fall. She reports that she was diagnosed with a “broken bone” in her leg but was unsure of which one. She had been unable to follow up in a clinic due to insurance issues which led to her multiple presentations. Additionally, the patient had a history of an unknown type of knee reconstruction on the affected knee one year prior.
ROS:
(+) R knee pain
Social Hx:
Tobacco use
Medical History
EtOH use disorder, hepatitis C, and tobacco use disorder
Surgical History
Right knee reconstruction 2020
Physical exam
Swelling and tenderness to palpation of the right knee with intact motor, sensation, and distal pulses. Full range of motion of right knee joint with noticeable varus laxity and a positive anterior drawer sign.
Imaging
X-ray performed in the ED was notable for moderate joint effusion but no visible fractures (image 1).
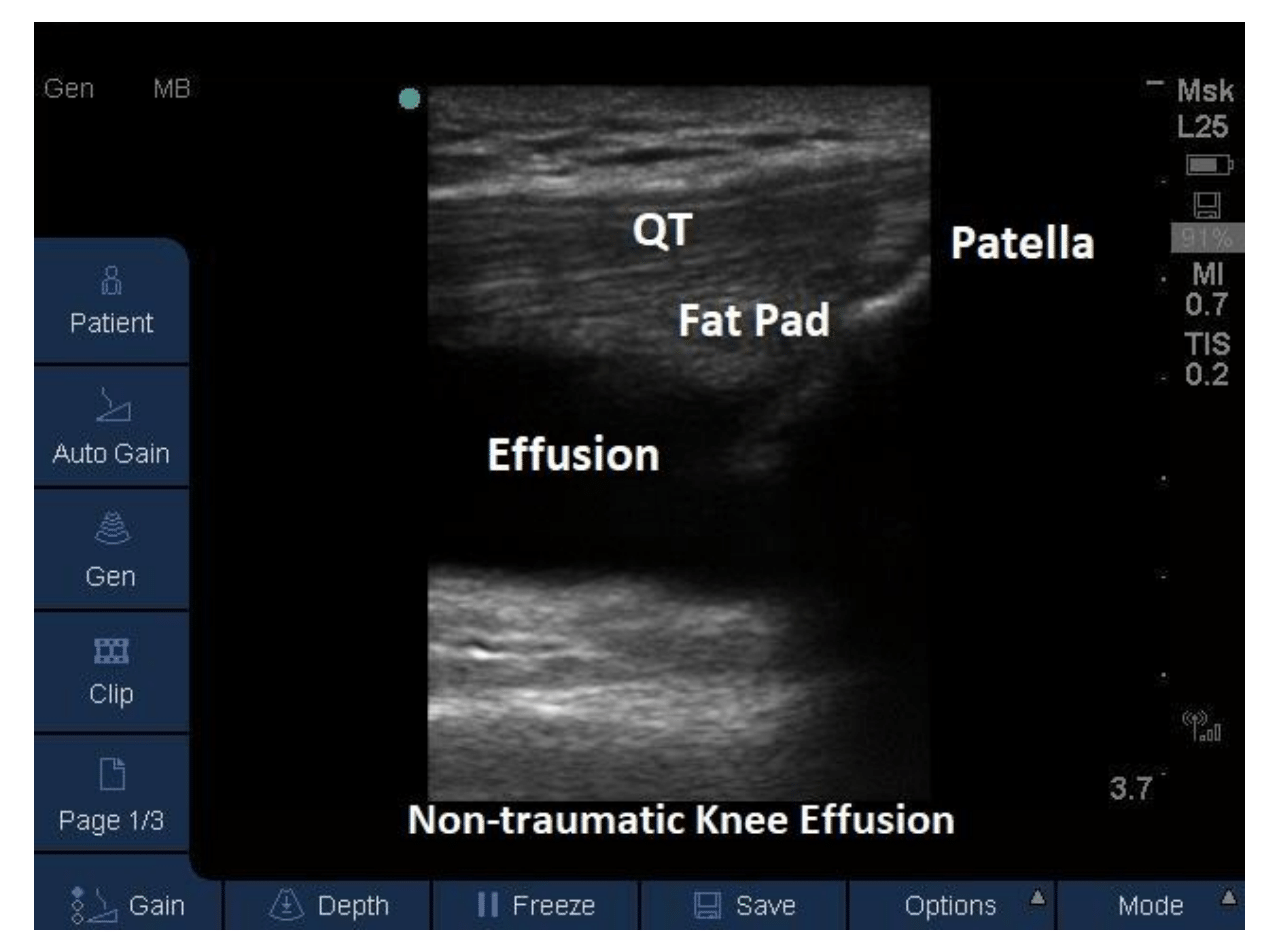
Given the patient’s exam and her inability to bear weight on the involved extremity there was high clinical suspicion for occult fracture. A POCUS was performed in the emergency department which was significant for visualization of three distinct layers from superficial to deep consisting of fat, serum, and red blood cells (image 2, video 1). The findings on US of LH suggested the presence of an occult tibial plateau fracture, therefore a CT of the knee was ordered.
Video 1
These suspicions were confirmed on CT which showed a non-displaced, non-depressed tibial plateau fracture (image 3) associated with a large lipohemarthrosis.
Management
Orthopedic surgery was consulted who recommended that the patient be placed in a hinged knee brace with no weight bearing for 12 weeks. There was no indication for acute surgical intervention. The patient was provided symptomatic relief with traditional rest/ice/NSAIDs/elevation and a 3-week outpatient follow up with orthopedic surgery was recommended. DVT prophylaxis with aspirin was also prescribed until orthopedic follow up.
How to evaluate a knee effusion step by step
First, you will have your patient lay supine and flex their knee to 30 degrees if tolerated. You can help your patient with this by placing a pillow behind their knee. Doing this helps by stretching some of the structures you want to evaluate, such as the quadriceps tendon. Flexing can also help some fluid into the suprapatellar recess which is the area you will be evaluating for effusion. An additional plug for ultrasound here: US is VERY good at assessing for fluid (image 4). Some studies even show that an effusion as little as 4 cc’s can be visualized on US.
Image 4
Next – which tools to grab for this exam. When picking a transducer, it is important to look at the size of the patient’s leg/knee. Traditionally a linear array transducer with MSK presets is utilized, but if the knee or effusion is large, you can get away with utilizing a lower frequency curvilinear transducer.
You want to start out by looking at a sagittal section of the knee at the midline. Place the transducer midline and just superior to the patella and slide the probe proximally to fully evaluate the suprapatellar pouch and its upper recesses (video 2).
Next you want to evaluate the lateral and medial borders of the patella and femoral condyles since we know effusions love to present themselves in these areas.
Throughout your evaluation you want to look for anechoic or hypoechoic collections of fluid representing effusions.
These collections can appear slightly echogenic secondary to fine particulate matter being mixed in (can be blood or purulent matter).
More relevant to our case, you will look for that parfait – a double or triple layered effusion to aid in finding a LH and ultimately a possible intraarticular fracture
Finally, scan the area of interest in transverse (also video 2)
See video 3 for an example of a normal quadriceps tendon
Video 2
Video 3
Pearls
As this case demonstrates, tibial plateau fractures can be subtle and can be missed on Xray. Thus, the pro tips for today’s lesson include:
Utilize ultrasound to evaluate for clues like LH that indicate an occult intraarticular fracture and warrant further imaging for your patient.
You can also visualize a fracture on a bony surface sonographically by looking for a “step” in the adjacent cortex (image 5).
Unfortunately due it’s central location within the joint the fracture could not be visualized in this case.
Happy Holidays!
References
Lyn E, Pallin D, Antosia RE. Knee and lower leg. In: Marx, JA ed. Rosen's Emergency Medicine: Concepts and Clinical Practice, 6th ed. St. Louis: Mosby; 2006: 620-621.
Aponte EM, Novik JI. Identification of lipohemarthrosis with point-of-care emergency ultrasonography: case report and brief literature review. J Emerg Med. 2013 Feb;44(2):453-6. doi: 10.1016/j.jemermed.2012.07.062. Epub 2012 Sep 13. PMID: 22981316.
McCaig L.F., Nawar E.W.: National Hospital Ambulatory Medical Care Survey: 2004 emergency department summary. Adv Data 2006; 372: pp. 1-29
Rippey J. Ultrasound for knee effusion: lipohaemarthrosis and tibial plateau fracture. Australas J Ultrasound Med. 2014;17(4):159-166. doi:10.1002/j.2205-0140.2014.tb00239.
Blog post edited by Dr. Michael Weaver, USF emergency medicine PGY-3