DVT in 1, 2, 3!
POCUS for Diagnosing Lower Extremity DVT in ED
Jennifer Shin, MD
Top Takeaways:
1. When performing a bedside DVT ultrasound, 3-point compression protocol is preferred and emphasizes areas at risk of DVT
2. Thrombus may be anechoic (acute) vs. echogenic (subacute, chronic)
3. Non-compressible? No echogenic clot? Color flow + Squeeze calf = Perform augmentation!
5. Treatment of DVT and what to do for a moderate/high-risk patient with negative DVT study = repeat scan
Why do We Care?
Deep vein thrombosis (DVT) is a thrombus that forms within the deep peripheral veins. Venous stasis, endothelial damage, or inflammation can lead to a hypercoagulable state. When the clotting cascade is activated along with aggregation of platelets and blood cells, a thrombus can form. The thrombus can be partial or a complete occlusion leading to venous stasis and possible ischemia to surrounding tissue. The DVT can dislodge and become a pulmonary embolism, which carries a high mortality rate. Also, DVT can cause chronic post thrombotic syndrome, which is a painful disorder caused by valvular compromise leading to chronic swelling. Identifying and treating is key to preventing these complications. Point of care ultrasound (POCUS) for DVT has great utility for the ED physician as it is a quick and non-invasive way to assess for DVT. Evidence has shown that ED physicians are able to perform this with the same accuracy as radiology performed (1). We will briefly discuss the indications of a DVT ultrasound, the anatomy of the lower extremities, different approaches for evaluation, and proper technique.
Indications:
Indications for use of point of care DVT ultrasound for the ED includes patients who present with leg swelling, painful extremities, or for concern for pulmonary embolism with concomitant DVT. POCUS for DVT evaluation has a sensitivity of 96.1% (95% CI 90.6-98.5%) and specificity 96.8% (95% CI 94.6-98.1%) (1).
Ultrasound Exam Protocols:
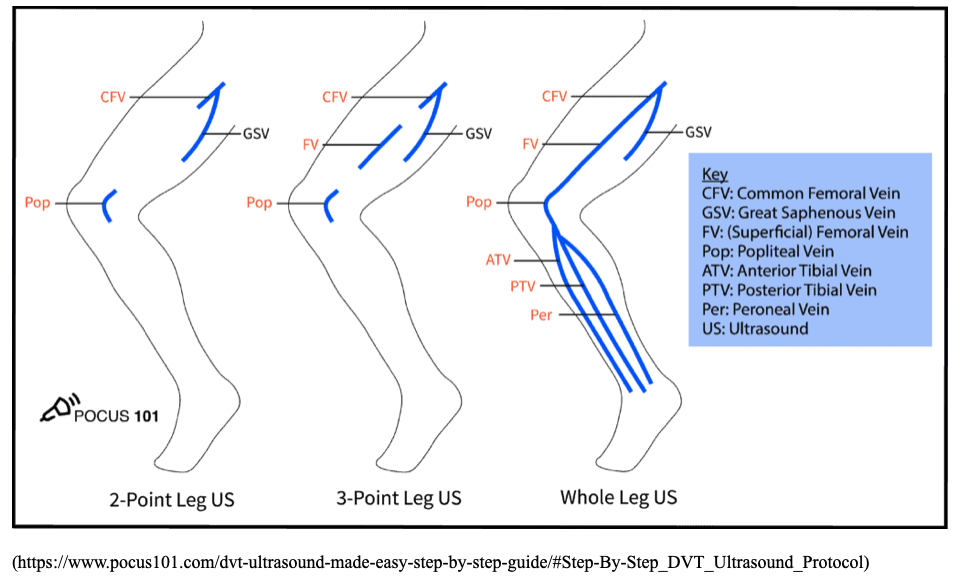
There are different protocols when using POCUS for DVT. DVTs can be evaluated using a 2-pont ultrasound, 3-point ultrasound or a whole leg scan. The 2-point ultrasound compresses the femoral vein 1-2 cm above and below the saphenofemoral junction and the popliteal vein. The 3-point ultrasound compresses the femoral vein 1-2 cm above and below the saphenofemoral junction, 1-2 cm above and below the bifurcation of the common femoral vein into deep femoral and superficial femoral vein, and the popliteal vein. The whole-leg DVT ultrasound scans the leg using compression, color Doppler, and pulse wave Doppler from the common femoral vein to the ankle. This is more commonly performed in the radiology dept.
The 3-point compression US protocol has been found to be more applicable in the ED setting with similar sensitivity and specificity to a whole leg scan. 3-point compression has shown a sensitivity and specificity of 100% (95% CI, 96.55%-100%) and 93.3% (95% CI, 87.72%-96.91%), respectively, in comparison with whole-leg compression ultrasound. Negative predictive value and positive predictive value were 100% and 92.11% (95% CI, 86.12%-95.64%), respectively, with an accuracy of 96.25% (3). Therefore, we will focus on the 3-point compression POCUS DVT study for this blog.
3-point Compression POCUS and Anatomy:
Next lets highlight the locations for the 3-point compression as well as the venous anatomy of the lower extremity. The 3-point compression focuses on the three regions that have higher turbulence and are at greatest risk for developing thrombosis. The veins of the lower extremity are classified according to their relationship to the muscular fascia and are in either the superficial or deep compartment. Deep veins lie beneath the muscular fascia and drain the lower extremity muscles. Most of the deep veins course along with their associated arteries. The deep veins of the lower extremity are: anterior and posterior tibial veins and peroneal veins, soleal and gastrocnemial veins that drain into veins in the calf and popliteal fossa, popliteal vein, femoral vein, deep femoral vein, common femoral vein, and external iliac vein.
The sites for the 3-point ultrasound include the saphenofemoral junction, femoral vein, and popliteal vein.
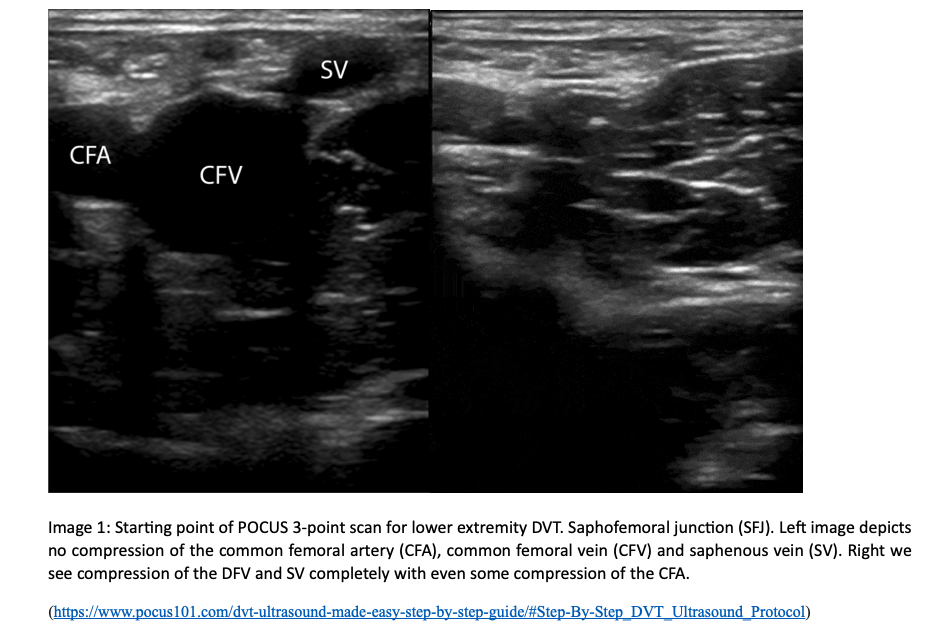
The most proximal point of our POCUS is the saphenofemoral junction (SFJ). For the first point of the scan, patient should be supine with the patient’s leg externally rotated and the knee flexed in a “frog-leg” position. Place the linear transducer transversely over the inguinal crease. The probe should be perpendicular to the skin with the indicator facing the patient’s right. Find the common femoral artery and common femoral vein (CFV). Proximal to the common femoral artery and vein, locate the SFJ as your most proximal point, which is 1-2 cm below the inguinal canal combining with the CFV.
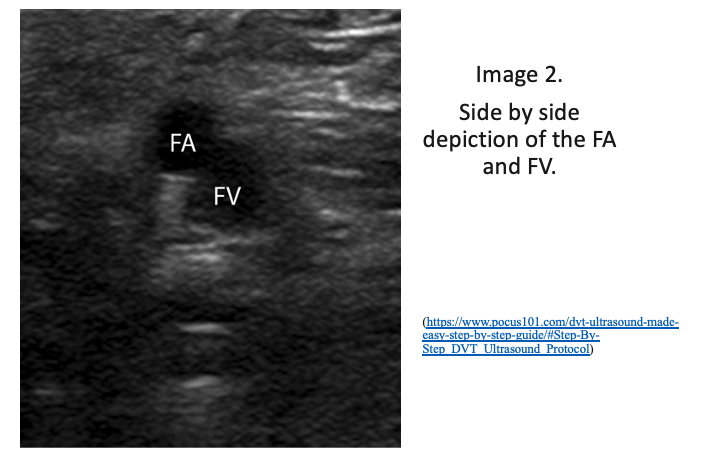
2. Continue to scan distally to locate where the CFV branches into the deep femoral vein and the femoral vein (previously known as superficial femoral vein). Remember the CFV will be medial to the common femoral artery. Compress the femoral vein distal to the bifurcation of the CFV at the SFJ. I like to compress until I cannot visualize anymore and the vasculature dives into the adductor canal. Firmly compress the ultrasound probe to assess if the vein compresses entirely.
3. The last location for the 3-point POCUS is the popliteal vein. Take your probe and place it into the posterior crease of the knee. The popliteal vein lies directly on top of the popliteal artery. You can have the patient lie on their belly, side, have them slightly bend the knee or frog-leg even for best positioning. Compress the popliteal vein. One of the most common reasons for a false negative DVT scan is incorrect identification of the popliteal vein! Remember, the popliteal vein is directly on top of the popliteal artery.
Pathology and Technique
At each location, compress the probe firmly into the skin until you see the vein compress completely. You may notice that the artery will also minimally compress as you assess the vein’s patency. If the vein is not compressible, this could indicate a DVT. You may not see an acute thrombus as they can be anechoic or hypoechoic. If the vein has echogenic material within the lumen, this can indicate a subacute or a chronic DVT. As the thrombus ages, it becomes more echogenic and pull away from the vein walls (see Clip 1).
If you cannot compress the vein completely, try augmentation with color and pulsed wave (PW) doppler (see Clip 2). Try also to turn from transverse to long. When you place the color doppler over the veins in question, there should be a homogenous increase in venous flow that fills the vein. If there is no increase in venous color flow, this could indicate a DVT. In deep venous structures, flow velocity varies with respiratory cycle and changes in intrathoracic pressure. Place the PW doppler over the veins middle and hit PW again. If there is a lack of variation in flow as the patient breathes, it can suggest an obstructive process.
These are advanced techniques but not technically challenging. Essentially it involves using color and pulsed wave doppler to assess for any filling defect or changes in wave form. Please see videos below under “additional info” to see how it’s done!
Clip 1. Right popliteal vein with large echogenic clot. Notice the hyper echoic texture as well as the central location, this indicates subacute chronic nature of the thrombus.
Clip 2. Popliteal vein and artery with color flow. The examiner was pushing hard enough to deform the popliteal artery without complete compression of the vein, concerning for thrombosis. There is also no visible flow in the vein with color doppler.
Treatment
A proposed DVT management algorithm is shown below (3). There has also been a study completed by Wells and colleagues for the management of DVT based on clinical probability: low, moderate, high. In patients with a LOW pretest probability on Well’s Criteria with a NEGATIVE DVT study do not need repeat testing. The negative predictive value was 99.7%. Thus, it rules out a DVT in patients in the low pretest probability group. In patients with moderate pretest probability and an initially negative DVT study, 17% developed a DVT on follow-up testing. Therefore, it is recommended that patient’s who fall into the moderate pretest probability group should get repeat ultrasound in 1 week. Patients who fall into high pretest probability had an incidence of DVT of 75% on initial ultrasound. Even if patients in this group have a negative DVT study, they should undergo further confirmatory testing (5).
Another study evaluates the incorporation of d-dimer with clinical probability and ultrasound. Tick and colleagues recommend obtaining a D-dimer in patients with moderate to high pretest probability of DVT if they have a negative DVT. If d-dimer is positive, the ultrasound should be repeated in 1 week. If they have a normal D-dimer, there is no need for a repeat ultrasound (7).
Summary:
Deep vein thrombosis is a thrombus that forms within the deep peripheral veins. A DVT can dislodge and become a pulmonary embolus, which carries a high mortality rate. Therefore, a bedside ultrasound to identify a DVT is an easy, quick, and noninvasive tool that provides significant utility in the ED setting. The sensitivity and specificity of the 3-point DVT ultrasound is similar to that of a whole-leg compression study. When scanning the lower extremities, the points of study include the saphenofemoral junction, femoral vein and popliteal vein. If the vein is fully compressible by firm pressure with the transducer, it is likely a negative study. However, if the vein is non-compressible, augmentation with color and PW doppler can be used to help differentiate acute vs subacute/chronic thrombi. Furthermore, a bedside DVT ultrasound can be used to guide treatment in conjunction with the Well’s criteria and D-dimer lab test.
Additional Info!
Check out these videos if you are interested in how to perform a 3pt compression DVT scan, augmentation with pulsed wave doppler for lower extremity DVTs:
POCUS - LE DVT - Updated by POCUS Geek
SinaiEMUltrasound more in depth including augmentation and respiratory variation.
Resources:
Pomero F, Dentali F, Borretta V, Bonzini M, Melchio R, Douketis JD, Fenoglio LM. Accuracy of emergency physician-performed ultrasonography in the diagnosis of deep-vein thrombosis: a systematic review and meta-analysis. Thromb Haemost. 2013 Jan;109(1):137-45. doi: 10.1160/TH12-07-0473. Epub 2012 Nov 8. PMID: 231384202.
Dehbozorgi A, Damghani F, Mousavi-Roknabadi RS, Sharifi M, Sajjadi SM, Hosseini-Marvast SR. Accuracy of three-point compression ultrasound for the diagnosis of proximal deep-vein thrombosis in emergency department. J Res Med Sci. 2019 Sep 30;24:80. doi: 10.4103/jrms.JRMS_1057_18. PMID: 31620179; PMCID: PMC6788177.
Lee JH, Lee SH, Yun SJ. Comparison of 2-point and 3-point point-of-care ultrasound techniques for deep vein thrombosis at the emergency department: A meta-analysis. Medicine (Baltimore). 2019 May;98(22):e15791. doi: 10.1097/MD.0000000000015791. PMID: 31145304; PMCID: PMC670901
Mazzolai L, Ageno W, Alatri A, Bauersachs R, Becattini C, Brodmann M, Emmerich J, Konstantinides S, Meyer G, Middeldorp S, Monreal M, Righini M, Aboyans V. Second consensus document on diagnosis and management of acute deep vein thrombosis: updated document elaborated by the ESC Working Group on aorta and peripheral vascular diseases and the ESC Working Group on pulmonary circulation and right ventricular function. Eur J Prev Cardiol. 2022 May 27;29(8):1248-1263. doi: 10.1093/eurjpc/zwab088. PMID: 34254133.
Schick MA, Pacifico L. Deep Venous Thrombosis Of The Lower Extremity. [Updated 2022 Sep 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
Wells P, Anderson DR, Bormanis J, et al. Value of assessment of pretest probability of deep-vein thrombosis in clinical management. Lancet 1997;350(9094):1795–8.
http://www.emdocs.net/risk-of-clot-when-imaging-says-not/