Managing Umbilical Cord Emergencies
We may not deliver many babies in the emergency department, but even at tertiary care centers with 24/7 OB coverage, sometimes babies decide to make their entrance into the world before arriving to the L&D floor. Emergency Medicine physicians need to be prepared to deliver a baby emergently and manage both common umbilical cord complications as well as life threatening cord emergencies.
Case #1
Mom was a 27 y/o G4P3 female who presented to the ED in labor and precipitously delivered a 7 lb 8.5 oz male. Baby had a nuchal cord with space for 1-2 fingers between the cord and neck. As the cord was reduced over the baby’s head, it ruptured and started spurting blood.
NUCHAL CORDS
A “nuchal cord” occurs when the umbilical cord is wrapped 360° around the infant’s neck and may be a single loop or multiple loops. Nuchal cords are quite common, occurring in 10-30% of fetuses, and can sometimes be diagnosed on prenatal ultrasound [1]. Risk factors for nuchal cord formation include polyhydramnios allowing for excessive fetal movement and long umbilical cords which more easily wrap around the baby’s neck [2].
Most nuchal cords do not cause significant complications but there are risks to the fetus given that the baby’s blood supply is wrapped around her airway. Strangulation syndrome can result in facial duskiness, petechiae, and subconjunctival hemorrhage. Direct cord compression can cause hypovolemia, decreased perfusion, and respiratory distress syndrome [1].
Management of nuchal cords
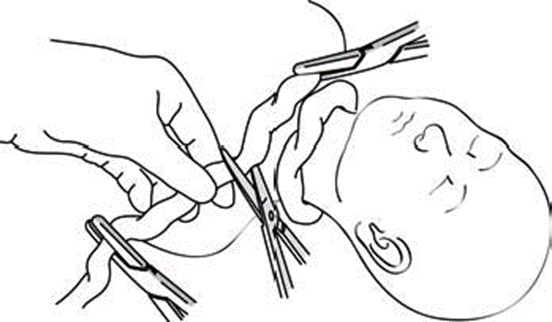
Baby’s head delivers with the cord around her neck – what do you do?
1) Is the cord relatively loose? If so, slip the cord over the baby’s head and proceed with delivering the body.
2) Is the cord tight? Clamp the cord in 2 places and cut in between clamps.
Image Source: https://medicalguidelines.msf.org/viewport/ONC/english/5-5-nuchal-cord-51417002.html
3) Did the cord just rupture as you attempted #1? DON’T PANIC
The umbilical cord needs to be clamped and cut anyway, but with a cord rupture, this process happens backwards with the “cutting” occurring first. So now you need to clamp. Start with clamping the section of the cord still attached to baby to avoid significant blood loss and then clamp the section attached to placenta. How often might you see a cord rupture? For an ED physician, probably once if ever in your career. Cord ruptures are rare, with only case reports published [4]. Increased risks of cord rupture include short cords, cord hematoma, and possibly gestational diabetes due to disruption of cord connective tissue weakening the tensile strength [5]. While you may never have to manage a ruptured nuchal cord, it is important to remember the steps to reducing both a loose and tight cord. Furthermore, be familiar with your ED’s L&D kit, and make sure you always have more clamps than you think you need.
Case #2
A 28 y/o G2P1 female at 37w gestation presents to the emergency department 1 hour after she started having abdominal cramps and felt a gush a fluid. “I think my water broke and I’m afraid the baby is coming out because I feel something in my vagina!” Manual exam is significant for a pulsating structure present in the vaginal vault.
Umbilical Cord Prolapse
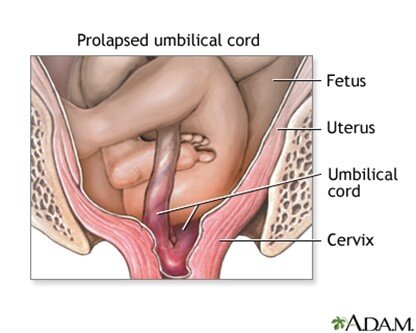
Umbilical cord prolapse occurs when the umbilical cord exits the cervix before the presenting fetal part (overt prolapse) or along with the presenting fetal part (occult prolapse). Cord prolapse occurs in approximately 0.5% of pregnancies and risk factors include prematurity / low birth weight and fetal malpresentation. Most prolapses occur within 1 hour of membrane rupture [6].
Cord prolapse is a true obstetric emergency due to resultant cord compression as the baby continues to descend through the birth canal, causing fetal hypoxia and bradycardia. Occult prolapse is a clinical diagnosis where a pulsating cord can be palpated or visualized in the vaginal introitus. Occult cord prolapse is diagnosed based upon fetal heart rate abnormalities [6].
Image Source: https://medlineplus.gov/ency/presentations/100193_4.htm
Management
1) Keep your hand in the vagina to elevate the fetal presenting part off the cord – until the baby can be delivered, you must prevent the fetus from compressing the cord (so sit on the bed and get comfortable).
2) Place mom in knee-to-chest position and ask her to try not to push or cough.
3) Get an OBGYN STAT! Definitive management is an immediate C-section and the fetus must be elevated off of the cord until delivery.
4) DO NOT TRY TO PUSH THE CORD BACK IN.
If time to C-section will be prolonged, for instance if the patient will need to be transferred for definitive obstetric care, infusion of 500-700 mL of saline into the bladder can elevate the uterus and may decompress the fetal part off the cord. Additionally, tocolytics can be used to slow contractions and stall labor until C-section delivery [6].
Although Emergency Medicine physicians may not have the same familiarity with obstetric emergencies as our OB colleagues, one skill we DO utilize daily is our ability to work as a team. In any emergent delivery, you need many coordinated hands and good communication skills to protect both patients, and luckily, this is something that is second nature for specialty.
References
[1] Peesay M. Nuchal cord and its implications. Matern Health Neonatol Perinatol. 2017;3:28. Published 2017 Dec 6. doi:10.1186/s40748-017-0068-7
[2] Sherer DM, Ward K, Bennett M, Dalloul M. Current Perspectives of Prenatal Sonographic Diagnosis and Clinical Management Challenges of Nuchal Cord(s). Int J Womens Health. 2020;12:613-631. Published 2020 Aug 10. doi:10.2147/IJWH.S211124
[3]https://medicalguidelines.msf.org/viewport/ONC/english/5-5-nuchal-cord-51417002.html
[4] Walker C, Ward J. Intrapartum umbilical cord rupture. Obstet Gynecol. 2009 Feb;113(2 Pt 2):552-4. doi: 10.1097/AOG.0b013e318193beaf. PMID: 19155954.
[5] Singh SD. Gestational diabetes and its effect on the umbilical cord. Early Hum Dev. 1986 Oct;14(2):89-98. doi: 10.1016/0378-3782(86)90114-3. PMID: 3792260.
[6] Boushra M, Stone A, Rathbun KM. Umbilical Cord Prolapse. [Updated 2020 Nov 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542241/
[7] https://medlineplus.gov/ency/presentations/100193_4.htm
About the Author
Dr. Jillian Kiely is a PGY-1 at USF Emergency Medicine. She attended Eastern Virginia Medical School (EVMS) in Norfolk, VA. Prior to medical school she completed a Masters in Public Health at Johns Hopkins Bloomberg School of Public Health and worked in pharmaceutical consulting.
This post was edited by Dr. Enola Okonkwo.