RSI Medication Choice and Patient Safety Study Demonstrates How Medical Students Can Get Involved with Research!
Tucker Maute, DO (LECOM) is currently a resident at Orlando Health. Prior to residency, he rotated with us in the ED at USF/Tampa General Hospital. Dr. Maute reached out to our faculty, as a medical student wanting to enhance his rotation and engagement with the program by assisting with research and completing a research rotation. Dr. Gillen reviewed several cases of peri-intubation morbidity and mortality when succinylcholine was used in the ED for crashing patients where rapid sequence intubation (RSI) was indicated. Dr. Wilson took a look at the case summaries that Dr. Gillen provided and realized that there was an opportunity for a broader manuscript exploring the safety profile and use of paralytic agents at our institution. The group met and devised a plan to review 7 years of ED rapid sequence intubation (RSI) data from our institution and create some proxies for how well those intubations went and whether there was some signal that, perhaps, one paralytic appeared safer than the other. The authors recognized that this was a retrospective study and, thus, only broad descriptions of patterns leading to potential hypothesis generation.
Succinylcholine, a depolarizing paralytic is widely used go to in the resuscitation bay. When there are perceived contraindications to sux, physicians sometimes go for non-depolarizing agents – like rocuronium and vecuronium – instead. With the significant boxed warnings in the succinylcholine package insert and potential contraindications, would it be safer to just use non-depolarizing agents like roc and vec?
Succinylcholine Package Insert Boxed Warnings
Recognizing significant potential for confounders in the retrospective study design, the authors hunted for signals of safety differences between the two groups of paralytics. Specifically: was there an all-cause mortality difference? Was sux used in patients that were later found to have defined contraindications to the drug that were not known when the patient was in extremis? Finally, were rescue airways used more often in one group of drugs compared to another? Here, we considered decision to utilize fiberoptic intubation after attempting direct or video laryngoscopy as a proxy for rescue airway use.
The advantage of a retrospective analysis is the ability to examine large data sets. Here, the authors had data available for 36,059 intubations in the ED over the study period. The majority of those intubations were done with sux (75%), confirming the popularity of the go-to drug. The other 25% of intubations were completed with non-depolaring agents roc and vec. There were 39/100,000 deaths that took place during RSI. There was actually a higher rate of mortality in the vec (75/200K)/roc group (230/100K), combined vec/rock (90/100K) compared to the sux group (22/100K). This study does not attempt to explain WHY – only to highlight the difference. While differences in drug safety might be responsible, perhaps airway operators are also choosing non-depolarizing agents in sicker patients with an a priori higher mortality at time of RSI.
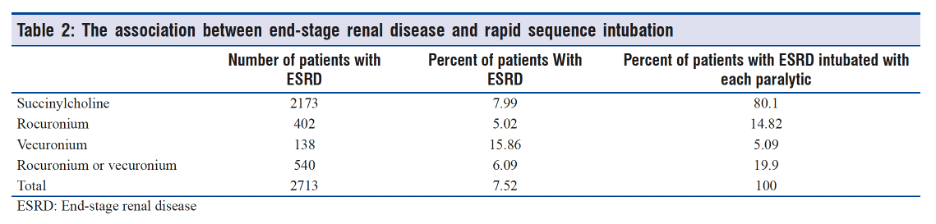
To get at the second question, is sux used in patients that have contraindications to sux, the authors reviewed chart data for evidence of ESRD or hyperkalemia documented soon after intubation. 2,713 of the 36,059 patients that underwent RSI had documented ESRD (7.52%). 8% of the patients intubated using sux had ESRD compared to 15% of patients undergoing RSI with roc, perhaps signifying some recognition in certain patients of the presence of ESRD. 6% of the patients intubated using vec had ESRD and, overall, vec was used less frequently across all sub-groups compared to roc.
Of note, hyperkalemia is a fairly common acute electrolyte derangement found amongst ED patients and, that information may not be known to an airway operator at time of intubation even if there is time for cursory review of the medical record. 1,696 patients had diagnosed hyperkalemia during the study period in the ED – representing high pretest probability for hyperkalemia in these patients. 845 patients had hyperkalemia diagnosed during the same ED encounter that they underwent RSI, signifying a potentially unknown contraindication to sux at time of intubation.
During the study period, 530 patients required fiberoptic intubation as a rescue maneuver after direct or video laryngoscopy attempt, representing 1.5% of all intubated patients (1,500/100K). 219 of the 27,186 patients intubated with sux required rescue airway (0.81% of all sux intubations). 311 of the 8,873 patients intubated with non-depolarizing agents roc and vec required rescue airway (3.5%). Again, the question becomes whether this is due to differences in drugs or some other variable influencing RSI drug selection (e.g. perhaps physicians chose non-depolarizing agents in patients that are sicker or more likely to have underlying contraindications to sux, making it more likely that a difficult airway will occur).
Succinylcholine is used 3Xs more often than roc and vec combined at our institution, likely improving the physician experience with the drug and increasing the sample size widely to include less critically ill patients. Even though sux has a more concerning risk profile, no adverse safety signal was observed in this retrospective analysis. As of right now, even with the knowledge that patients may have unknown ESRD or undiagnosed hyperkalemia at time of intubation, there is not a compelling argument to move away from the use of succinylcholine.
This study provides an example of how medical students can become involved in research projects at USF EM, leading to a manuscript publication. In addition, this paper serves as an example for how to parlay case reports into more systematically useful data that can be used to change clinical practice and lead to publication as more and more journals back away from publishing single case reports or case series without a quality or patient safety theory. While there was not a signal for patient harm in the succinylcholine group, the retrospective analysis allows us to confirm that our overall clinical choices between the two drug classes appears safe.
About the Authors
Dr. Gillen is Director of Emergency Medicine Education for USF and has served on the core faculty since 2008. Outside of work he is a proud father, dogfather, grandfather and the lucky husband of Marlene Gillen.
Dr. Wilson is a core faculty member for USF EM and, as research director, coordinates multiple research studies across TGH/USF. He also serves as the Associate Medical Director of the Emergency Department at TGH and is the Medical Director for the Clinical Decision Unit.
Post edited by Dr. Enola Okonkwo