The ACTIV-4 Trial aims to reduce venous thromboembolism (blood clot) risk in patients with covid-19 with apixaban or aspirin.
Operation Warp Speed is the federal government funded effort to rapidly develop vaccines and therapeutic modalities to treat, prevent, or minimize side effects of Covid through the Accelerating Covid-19 Therapeutic Interventions and Vaccines (ACTIV) protoocols. I serve as the site principal investigator for the ACTIV-4 trial at the University of South Florida, Tampa General Hospital. In this trial, we will randomize patients leaving the emergency department (ED) with a new diagnosis of Covid to receive apixaban [Eliquis], aspirin, or a placebo in order to see if we an reduce blood clots in Covid patients using medication. Our team will begin enrolling patients early in December 2020 (thanks to the leadership of Tiffany Vasey, ARNP, Ashley Bader, RN and Rachel Karlnoski, PhD).
There is a 8–30% risk of a blood clot (usually starting in the leg — a DVT — and/or moving to the lung — a PE) in patients with Covid. This risk seems to vary depending on how sick a patient is during their Covid course(patient that go home likely have a risk closer to 8-10% while patients admitted to the ICU may have risk closer to 30% for forming a clot). Even more alarming, these percentages are for what we refer to as “symptomatic” DVT/PE — meaning the patient had to complain about something or something in the physical exam or diagnostic testing had to suggest that the patient may have a DVT/PE. If patient’s underwent ultrasound screening (daily scans of the leg vasculature to look for silent clots),the rate of DVT appears to be as high as 70% in this population!
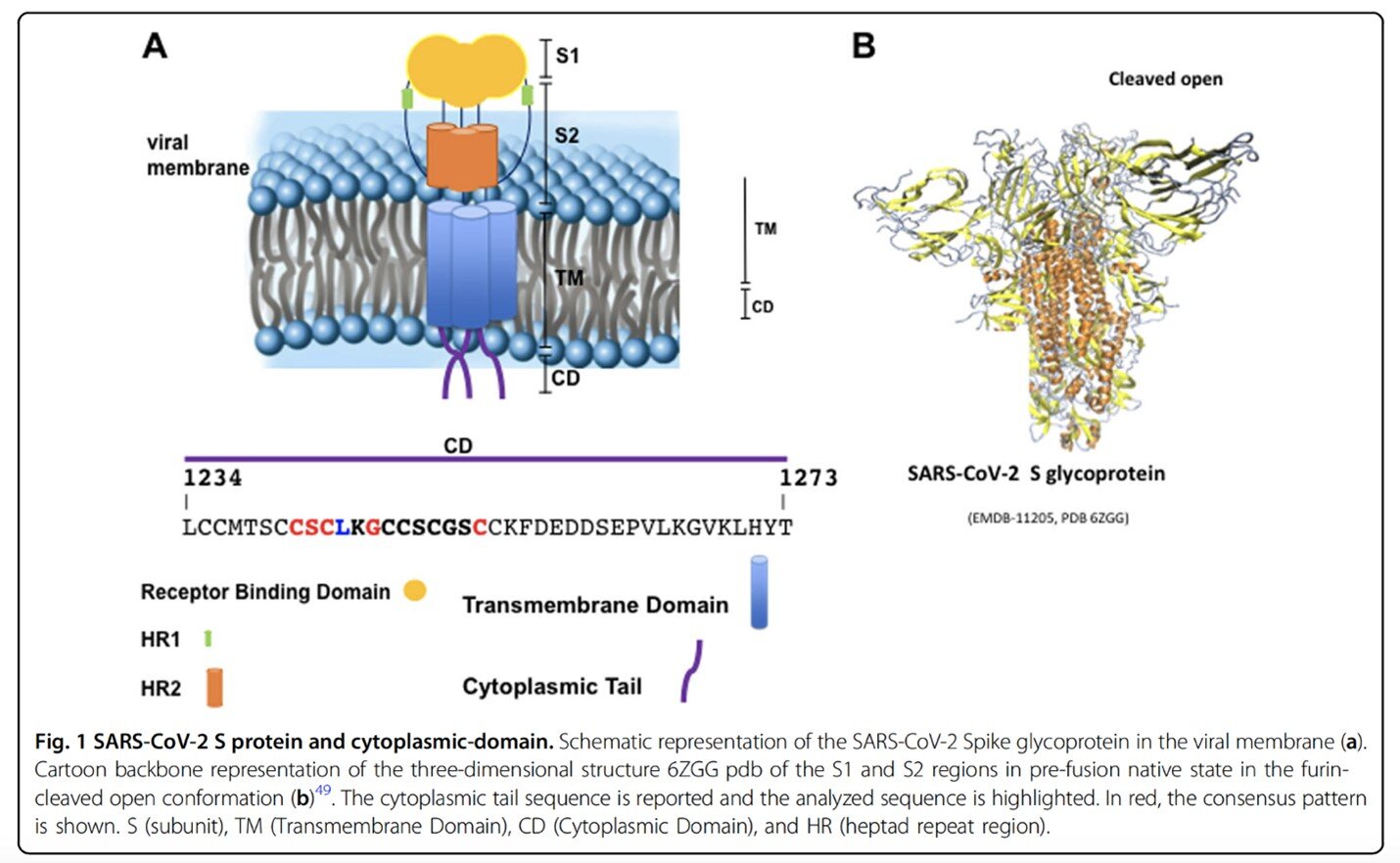
Why do we see increased clotting in patients with Covid? Ah, well, it seems to go back to that Spike protein (S protein) that we have heard about in relation to vaccine development (mRNA vaccines create Covid S protein), treatment targets (monoclonal antibodies target Covid S protein), and now, apparently, pro-coagulation (the propensity to form clots). How?
A very important paper was published in Cell Death and Discovery (a Nature journal) on November 27, 2020 (Buovino and Melino)that outlines proposed mechanism of clotting via the Covid Spike protein. The S protein is a three blade propeller with 4 functional sites.
These researchers isolated a genetic sequence of the Spike Protein called the CAF-motif that is also found in coagulation factor X and some other human pro-coagulopathic proteins (e.g. von Willebrand factor, platelet endothelial aggregation receptors) and also some pro-thrombin venom toxins (snake venom is often coagulopathic). The presence of the CAF-motif on the Covid surface Spike protein explains how the virus causes increased clotting in patients infected with the virus. The CAF-motif may also mean that DVT and PEs may occur more frequently in patients with Covid but, the similarity of CAF-motif to arterial side clotting agents (e.g. platelets) might mean that strokes and myocardial infarctions (heart attacks) may also occur more frequently in patients with Covid.
In addition to this virus-specific route of coagulability, all inflammatory states secondary to infection can result in clotting driven by IL-6 and leading a run away cascade increasing levels of inflammatory markers including ESR and CRP as well as higher levels of D-Dimer (elevated in patients with VTE). The virus also targets ACE-2 receptors (which is why early research considered ACE-Inhibitors blood pressure medications as a potential treatment target but that did not pan out) found on endothelial cells in blood vessels — thus leading to cell death and disruption of those cells and release of markers that promote further clotting.
Apixaban [Eliquis] is in a class of medications that have been around for about a decade called “Factor Xa Inhibitors”. Factor Xa inhibitors can usually be identified in their generic name by the “xa” (e.g. apiXAban, rivaroXAban). The medication was initially approved to reduce the risk of stroke in patients with atrial fibrillation (ARISTOTLE, 2011) and later expanded for the treatment and secondary prevention of DVT and Pulmonary Embolism (AMPLIFY, 2013). Different doses of Apixaban are used to treat DVT/PE or prevent DVT/PE. There is not definitive data for whether using an anticoagulant (a blood thinner) is helpful in reducing the risk of blood clots in patients with Covid-19. There are different doses of Apixaban available (e.g. 2.5mg, 5mg) and both will be tested in the study. In addition, Aspirin will also be studied as this old medication is an anti-platelet agent and works differently than Apixaban.
USF/TGH will begin enrollment of patients in December. The ACTIV-4 protocol can be found on the NIH website.
STUDY DESIGN
Patients 40–80 years old or older that present to the ED with mild-moderate Covid symptoms and are able to be discharged home will be undergo an informed consent process and then enrolled into the trial.
INCLUSION: Patients that are eligible to participate will have a positive Covid PCR test within last 14 days, be 40–80yo, have a phone, and not be pregnant.
EXCLUSION: Patients already on anticoagulation, pregnant/lactating patients, patients with active cancer, patients with high bleeding risk, patients with platelet count < 100,000/uL, CrCl < 30ml/min, hospitalized
A D-Dimer and CRP lab test will be conducted for each patient (as well as standard creatinine and platelet count measurements). The magnitude of D-dimer level and CRP elevation have been associated with worse clot burden/risk of clot in Covid.
The patients will be randomized to one of 4 arms in the trial — Apixaban 5mg, Apixaban 2.5mg, Aspirin 81mg, or a placebo. This is a double-blind study. That means that the researchers will not know which drug the patient is taking, nor will the patient. Each patient will take two pills each dose. The medication will be mailed to the patient after discharge from the ED.
The first principal of medicine is to do no harm. Anytime we conduct an anticoagulant study, there must be analysis of whether or not bleeding events are increased in the study arm. Major and clinically relevant non-major bleeding events will be recorded.
This is a prospective observational study — meaning the patient will take the drug/placebo and the study team will observe the patient for 45 days via repeated phone calls to look for the occurrence of the primary composite endpoint — DVT/PE, strokes or myocardial infarctions, or any hospitalizations related to heart, lung or vascular issues during the study period. Research during the era of Covid continues to push deadlocked boundaries that seemed stuck in quicksand prevous to the pandemic. In this trial, phone calls will be used for all patient visits to minimize further physical contact between research staff and a Covid+ patient. While a physician may begin the consent process in the ED (patient hears about the study and views a video), the process can be completed after discharge so that the patient does not have to wait for all laboratory testing to result before returning home.
Not all patients will be willing to take medication or may not meet all inclusion criteria — those patients will be offered enrollment into an observational registry study. Collected blood samples will also be stored for future analysis of potential pro-inflammatory, pro-coagulopathic biomarkers for Covid-19.
Patients that do enroll into the full study will have study drug overnight mailed to their house. The first follow-up study call will occur 24 hours after the package is mailed out to ensure receipt of drug. Patients will then be called weekly for 75 total days after enrollment (45 days for trial, additional 30 days for safety — do no harm!).
The observation period will be 45 days, unless a patient undergoes any of these events: hospitalization, DVT/PE, MI, stroke, arterial clot, death, major bleeding, new indication to start anticoagulation.
Currently, we already consider (with much consternation) whether a patient discharged with Covid should begin anticoagulant treatment. Whether placing these patients on an anticoagulant patient is a burning question where we face clinical equipoise (unknown answer) — just the right conditions for a clinical research trial.
References
ABOUT THE AUTHOR
Jason Wilson, MD is a core faculty member for USF EM and, as research director, coordinates multiple Covid research studies across TGH/USF.
Post edited by Enola Okonkwo, MD.