SVT on the ECG!
Arrhythmia management is one of the things I really love about emergency medicine. There’s something satisfying about slapping the defibrillator pads on a patient and analyzing an ecg rhythm. I thought I would share a recent lecture I gave on SVT during USF Conference and review some of the common ecg findings and pitfalls associated with this arrhythmia. In the full lecture below, you’ll learn more about SVT and the management of this condition.
Dr. Okonkwo discusses SVT during this lecture originally presented at USF on 9/16/20.
Technically speaking, SVT includes any arrhythmia that originates above the Bundle of His - this would include etiologies such as afib and flutter. However, from an ER perspective, when we use the term SVT, we are not talking about afib or flutter. We are usually using this term synonymously with AVNRT (AV nodal reentrant tachycardia) though there are certainly other types of “SVT”. For more on AVNRT and other forms of SVT, check out the lecture!
Let’s review 5 ecg findings you may see in SVT.
1) It’s Fast.
This is the SVT that we all know and love. This is the ecg that shows up on exams and the ecg that the triage nurse generally recognizes and leads to the patient being whisked off to the resuscitation bay. By definition, supraventricular tachycardia must be fast. This rhythm is usually narrow since it originates above the ventricles. However, it is possible for SVT to have a wide complex in the presence of a pre-existing bundle branch block, rate related aberrant conduction, or an accessory pathway. An example of a wide complex SVT will be reviewed later in the blog.
2) There are No normal p waves.
The absence of normal p waves are one of the things that typically define SVT. With a good eye though, you may see retrograde p waves which can create a pseudo R’ in V1 and pseudo s wave in inferior leads secondary to retrograde p waves. Check out the retrograde p waves in this ecg.
3) SVT can create scary looking ST depressions and avR elevation.
ECGs with avR elevation and diffuse depression immediately make me worry about ischemia associated with a proximal LAD lesion or other scary things like aortic dissection. However, in the setting of SVT, avR elevation and diffuse ST depression are common findings and do NOT correlate with CAD unless they persist following restoration of sinus rhythm. Notice the elevation in avR and the diffuse ST depression that is demonstrated in this ecg.
4) SVT may demonstrate a wide complex if there is an underlying bundle branch block or accessory pathway.
In regards to wide complex SVTs, It is very difficult to tell the difference between a wide complex SVT and ventricular tachycardia. Multiple algorithms and tips exist, but the bottom line is that these approaches are not reliable and it is usually safest for your patient to assume that the wide complex is ventricular tachycardia and treat it as such. Realistically, you may be dealing with SVT with an underlying bundle branch block or SVT with an accessory pathway such as an antidromic WPW pathway. Here’s an example of a wide complex SVT that is difficult to distinguish from ventricular tachycardia.
5) SVT may cause a pseudoelectrical alternans pattern.
Pseudoelectrical alternans has been reported in SVT. This would look much like the ecgs seen in tamponade with alternating voltages. The overall voltage of pseudoelectrical alternans is relatively normal in SVT as opposed to true tamponade. Of course, if I ever see this pattern my first thought would be to put an echo on the chest and look for effusion. In the setting of SVT related pseudoelectrical alternans you would not expect to see pericardial fluid.
And now, let’s review a few SVT pitfalls!
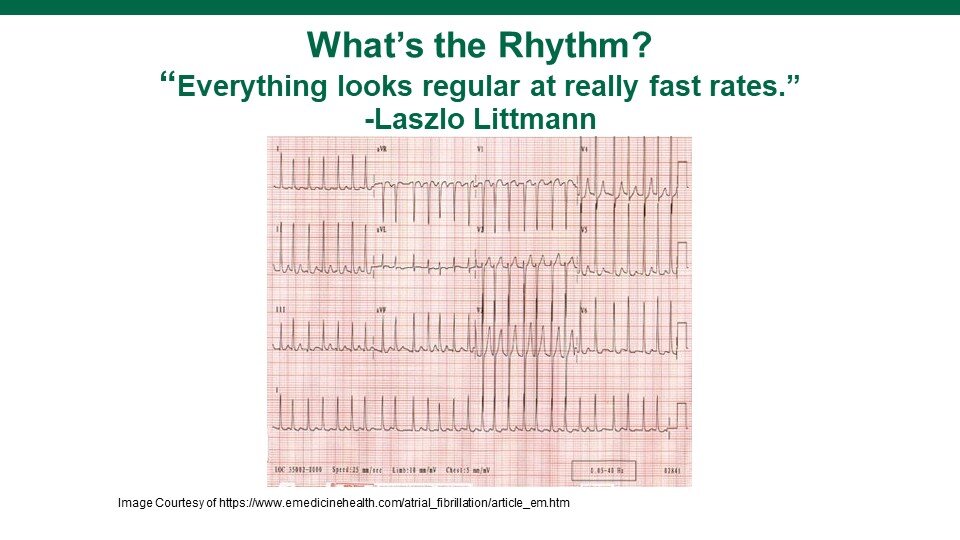
Remember that at really fast rates, everything looks regular. This is one of the key teaching points I took from Dr. Littmann and this knowledge bomb has helped me time and time again. Look at this ECG which initially looks like SVT. When examined closely, it is more likely afib given the slight irregularity that can be appreciated.
Atrial fibrillation with rapid rate which can be mistaken for SVT.
Be paranoid about atrial flutter because flutter waves like to hide! Atrial flutter can mimic both sinus tachycardia and SVT. The first ECG below was mistaken for SVT and it’s easy to see why. There’s really nothing about that initial ecg that would make me think flutter other than the rate. Once the patient was given Adenosine, flutter waves were revealed. The second ECG is a patient who was initially thought to be in SVT. On closer review of the rhythm, p waves can be identified in V2. Thus, the patient was either having sinus tachycardia or atrial flutter. Ultimately, the patient was found to have flutter. The third ECG below is patient number 2 again. I’ve simply circled the hidden p waves that I marched out with fancy $10 calipers. One last final atrial flutter ecg is included. In this ecg, flutter was actually mistaken for sinus tachycardia on initial review. However, notice that the p waves in the inferior leads are inverted. Sinus does not produce inverted p waves in the inferior leads. This is a big clue that you are dealing with a rhythm that originates somewhere other than the sinus node.
Atrial flutter which looks like SVT on this ecg. Flutter waves were not visible until adenosine given.
Atrial flutter initially thought to be SVT. Note the p waves visible in V2.
Flutter p waves marched out.
Atrial flutter with inverted p waves marched out.
Sinus tachycardia can easily be mistaken for SVT at rapid rates. The patient below was brought in via EMS with an identical rhythm strip. Because of her fast rate, she was given adenosine. The patient clearly has p waves and likely was in sinus rhythm the whole time. Remember that the max heart rate is 220 minus the patient’s age. Many patients can have HRs as high as 200 even in sinus!
Sinus tachycardia mistaken for SVT.
Lastly, the most important pitfall to avoid is don’t assume that a wide complex tachycardia is SVT. You and your patient will be safest if you assume that wide complex tachycardias are ventricular tachycardia and treat it as such!
I hope you’ve enjoyed the post! Check out the lecture and email me with any questions! Special thanks to all of my favorite educators in cardiology (Drs. Laszlo Littmann, James Bower, Troy Leo, Todd Haber, Amal Mattu, and the crew at Life in the Fast Lane)!
About the author
Dr. Okonkwo is the Assistant Program Director at USF. She attended medical school at Indiana University and completed her emergency medicine residency training at Carolinas Medical Center in Charlotte, North Carolina.