TICK ALERT – Rocky Mountain Spotted Fever is On the Rise!
Angela Tavolieri, Vincent Costers, Marco Gerges, Naveen Perisetla, Enola Okonkwo
Rocky Mountain Spotted Fever (RMSF), also known as spotted fever rickettsiosis, is a disease that is poised to fool clinicians from the start and if untreated, can be deadly with a mortality rate as high as 30% [1]. Even its name is a misnomer. It is most common in the southeastern and midwestern United States with very few cases originating in the Rocky Mountains. According to the CDC, Arkansas, Missouri, North Carolina, Tennessee and Virginia are responsible for over 50% of cases [2].
Annual Incidence (per million population) of reported spotted fever rickettsiosis - United States 2019
RMSF is the most common fatal tick disease in the United States [3]. While not home to the majority of RMSF cases, Floridians are not free from contracting this disease and it wasn’t long ago a presumed case was identified in our ED triage.
PRESENTATION
Patients present with a nonspecific viral-like syndrome which may include fever, headache, cough, myalgias, and gastrointestinal complaints. Two to five days after the fever, a macular rash may appear on the wrist and ankles with eventual spread to the trunk, palms, and soles [4]. Many consider the presence of the palmar rash a hallmark in the diagnosis of RMSF, but this finding may be absent in up to 20% of patients and often does not appear until later in the progression of the disease [5]. As the disease progresses, RMSF can lead to meningoencephalitis and patients may exhibit signs such as lethargy, seizures, and confusion. Around 10% of Rocky Mountain Spotted Fever cases will require hospital admission [6]. A study looking at the predictors of prognosis in hospitalized patients with RMSF show that elevated serum Cr, increased age, increase levels of AST, increased levels of bilirubin, decreased serum sodium and platelet count, and presence of neurological involvement all were associated with increased mortality rate. Furthermore, the presence of renal failure was ”strongly associated with death” in these patients [7].
Differential Diagnosis
With climate change, the range of the American Dog Tick is expanding both to the West and North leading to new endemic areas of Rocky Mountain Spotted Fever. This leads to increased missed diagnosis by exclusion of RMSF based on its historical distribution. In addition, in newly endemic areas, physicians may be unaware of standard treatment practices. As many as 25% of EM physicians in endemic areas are unclear of the correct antibiotic in children (Doxycycline) and many physicians still rely on development of a rash before initiating treatment. Current guidelines recommend treatment with Doxycycline as soon as RMSF is on the differential, regardless of rash as treatment within 5 days of symptom onset has a substantial mortality reduction [9].
“If you don’t think about it, you can’t diagnose it.”
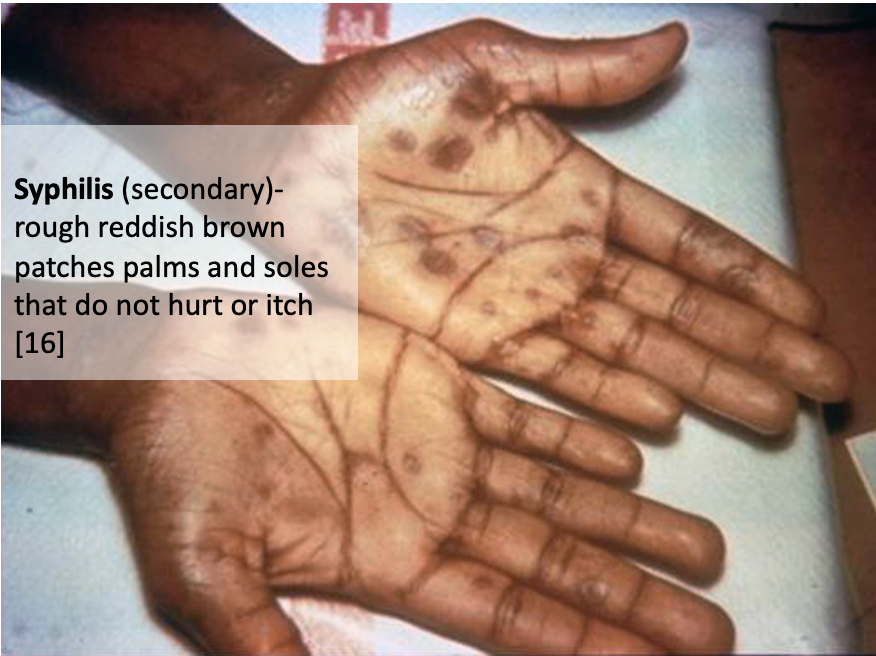
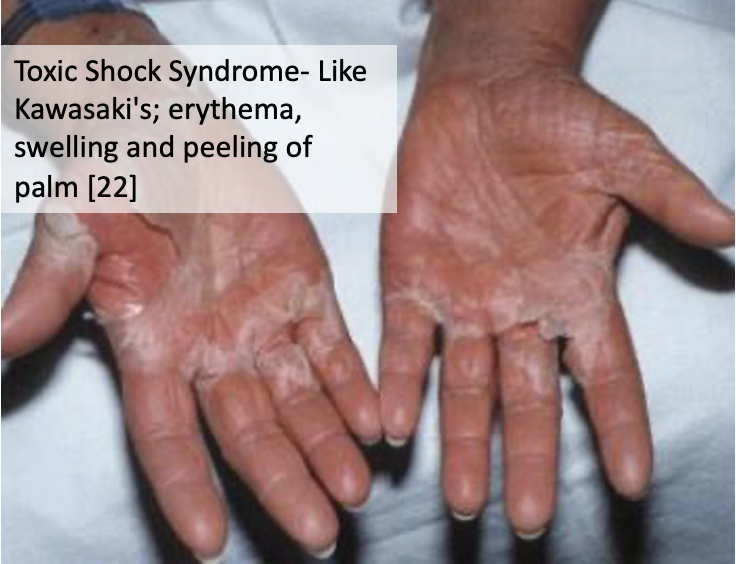
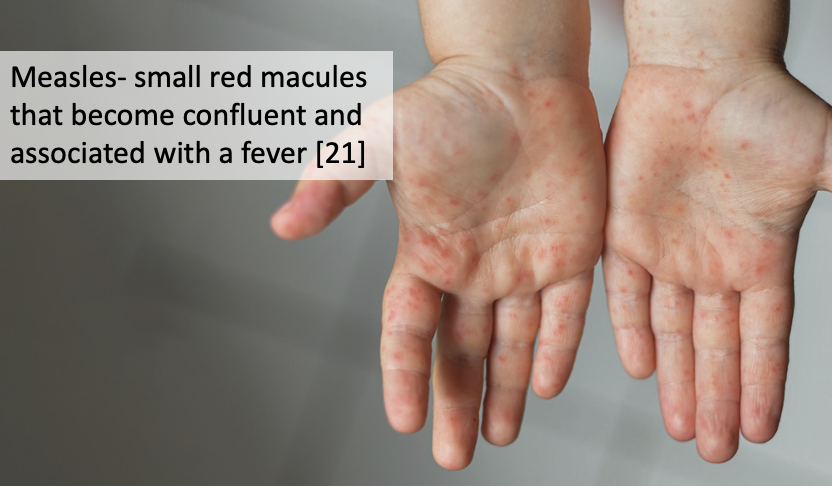
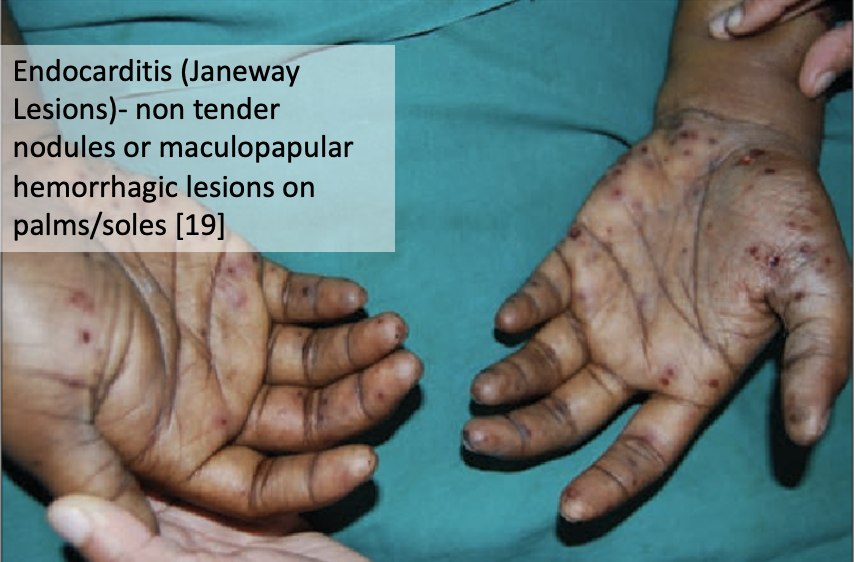
Below is a brief differential for rash on the palms. It is quickly apparent that many of these rashes are nearly identical in appearance. In recent years, cutaneous manifestations of Covid-19 is another consideration to keep on your differential [10] Determining the etiology of a rash in the ER is not easy! It’s important if the history is at all suspicious for tick exposure or if secondary symptoms are present, to initiate Doxycycline therapy before a final diagnosis is made to lower morbidity and mortality.
Check out the below link for more information on cutaneous manifestations of COVID-19!
TREATMENT
According to expert recommendations, first line treatment of RMSF for non-pregnant adults is Doxycycline 100 mg BID, PO or IV for stable patients for at least 7 days inclusive of at least 3 days after the last documented fever. This is based off clinical experience since there are no control trials to suggest alternative therapy durations [11]. In critically ill patients, a loading regimen of Doxycycline 200 mg IV has been utilized by many clinicians [12]. The only alternative available is Chloramphenicol, but Tetracyclines still remain first line treatment since the case fatality of Chloramphenicol monotherapy versus Tetracycline monotherapy was significantly worse (7.7 versus 1.6; odds ratio 5.5; 95% CI, 3.9- 7.7) [13]. Timely administration of Doxycycline is key to successful RMSF treatment. A study comparing fatal and nonfatal RMSF cases found that “Doxycycline was initiated significantly later in fatal cases (median, day 7) than nonfatal cases (median, day 3) [14].
In patients presenting with non-specific CNS symptoms, such as fevers of unknown origin with meningismus, it would be crucial to start broad antimicrobial and antiviral coverage following an LP, but also add Doxycycline to the regimen if there is any clinical concern for RMSF.
Also, empiric broad spectrum antibiotics, blood cultures and IV fluids should not be withheld in toxic appearing patients who meet SIRS criteria even if the clinician is attributing their presentation solely to RMSF. Sepsis protocol should be initiated for these patients as there is substantial clinical overlap between advanced cases of RMSF and sepsis from other causes, especially when the typical RMSF rash is not present.
The American Academy of Pediatrics recommends Doxycycline as first line treatment for children at a modified dose of 2.2 mg/kg BID for children under 45 kg and the normal adult dose for children above 45 kg. Even in cases of Doxycycline allergy, desensitization is typically recommended as the only available alternative agent, chloramphenicol, has a much higher treatment failure rate compared to Doxycycline.
RICKETTSIAL INFECTIONS ARE LIKELY ON THE RISE IN FLORIDA
The number of RMSF cases seem to be on the rise in Florida over the last 20 years. The recent Covid-19 pandemic has also made an impact on rising Ricketssial infections as social distancing efforts has resulted in increased outdoor activities such as hiking which makes people more prone to tick exposure. As a result, there is an expected surge in ticks and tick-borne related illness in Florida.
This actual incidence of RMSF in Florida is suspected to be higher than reported due to underreporting. The CDC requires that once a diagnosis of RMSF is confirmed, it should be reported to the local health department within a 24-hour period under the category of Spotted Fever Rickettsiosis (SFR) which includes RMSF, Rickettsia parkeri rickettsiosis, Pacific Coast tick fever, and rickettsial pox.
BIZARRE FACT ABOUT RMSF
RMSF can affect dogs as well. The dog tick is actually the most common vector. Some cases of RMSF occur within a cluster of family members and can even involve Fido, the family dog.
TAKE HOME MESSAGE
RMSF is a rare condition in Florida but is potentially fatal if unrecognized. Therefore, it is important that Florida-based practitioners understand how to recognize and treat Rocky Mountain Spotted Fever [15].
ABOUT THE AUTHORS SECTION
This post was written by USF Medical students and Emergency Medicine physicians.
REFERENCES
1. Dalton, M.J., et al., National surveillance for Rocky Mountain spotted fever, 1981-1992: epidemiologic summary and evaluation of risk factors for fatal outcome. Am J Trop Med Hyg, 1995. 52(5): p. 405-13.
2. Rocky Mountain Spotted Fever (RMSF). 2021; Available from: https://www.cdc.gov/ticks/tickbornediseases/rmsf.html.
3. RMSF: deadly, but preventable. 2019; Available from: https://www.cdc.gov/ncezid/dvbd/media/rmsf.html.
4. Phillips, J., Rocky Mountain Spotted Fever. Workplace Health Saf, 2017. 65(1): p. 48.
5. Blanton, L.S., The Rickettsioses: A Practical Update. Infect Dis Clin North Am, 2019. 33(1): p. 213-229.
6. Patel, S. Rocky Mountain Spotted Fever (RMSF) Treatment & Management. 2021; Available from: https://emedicine.medscape.com/article/228042-treatment.
7. Conlon, P.J., et al., Predictors of prognosis and risk of acute renal failure in patients with Rocky Mountain spotted fever. Am J Med, 1996. 101(6): p. 621-6.
8. Helmick, C.G., K.W. Bernard, and L.J. D'Angelo, Rocky Mountain spotted fever: clinical, laboratory, and epidemiological features of 262 cases. J Infect Dis, 1984. 150(4): p. 480-8.
9. Krawiec, C., et al., Impact of a Severe Rocky Mountain Spotted Fever Case on Treatment Practices at an Academic Institution Within a Nonendemic Area. Wilderness Environ Med, 2021. 32(4): p. 427-432.
10. Daneshgaran, G., D.P. Dubin, and D.J. Gould, Cutaneous Manifestations of COVID-19: An Evidence-Based Review. Am J Clin Dermatol, 2020. 21(5): p. 627-639.
11. Biggs, H.M., et al., Diagnosis and Management of Tickborne Rickettsial Diseases: Rocky Mountain Spotted Fever and Other Spotted Fever Group Rickettsioses, Ehrlichioses, and Anaplasmosis - United States. MMWR Recomm Rep, 2016. 65(2): p. 1-44.
12. Cunha, B.A., Clinical features of Rocky Mountain spotted fever. Lancet Infect Dis, 2008. 8(3): p. 143-4.
13. Holman, R.C., et al., Analysis of risk factors for fatal Rocky Mountain Spotted Fever: evidence for superiority of tetracyclines for therapy. J Infect Dis, 2001. 184(11): p. 1437-44.
14. Regan, J.J., et al., Risk factors for fatal outcome from rocky mountain spotted Fever in a highly endemic area-Arizona, 2002-2011. Clin Infect Dis, 2015. 60(11): p. 1659-66.
15. Levin, M.L., et al., Clinical presentation, convalescence, and relapse of rocky mountain spotted fever in dogs experimentally infected via tick bite. PLoS One, 2014. 9(12): p. e115105.
16. https://www.cdc.gov/std/syphilis/images/rash-palmar.htm
17. https://www.cdc.gov/hand-foot-mouth/about/signs-symptoms.html
18. https://www.cdc.gov/rmsf/healthcare-providers/signs-symptoms.html
19. I. Reddy, S. Gowrishankar, Janeway Lesions – revisted, Indian Journal of Dermatology, Venereology, and Leprology, 2013.
20. Adya KA, Inamadar AC, Palit A. The Strawberry tongue, What, how and where? Indian Journal of Dermatology, Venereology, and Leprology, 2018;84:500-505
21. https://www.choa.org/medical-services/infectious-diseases/measles
22. https://rmi.edu.pk/disease/toxic-shock-syndrome
23. https://www.wfla.com/news/tick-population-expected-to-surge-and-theyre-carrying-more-than-lyme-disease-researchers-say/