Maximizing the Simulation Experience: How to Get the Most out of Hybrid Learning as a Learner and Educator
Dr. Nicole Rettig
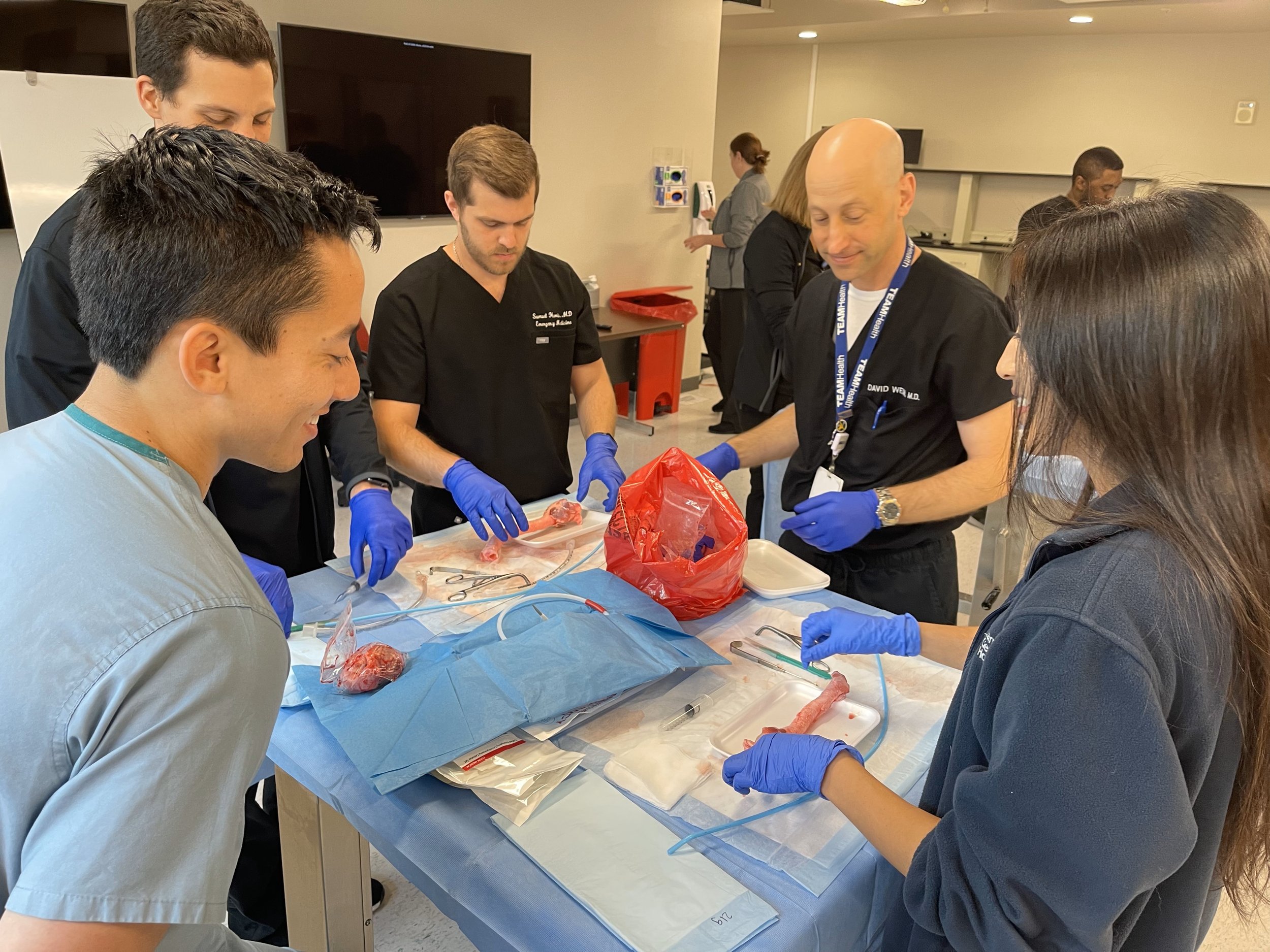
Clinical simulation can help improve quality and patient safety in healthcare. “Hybrid learning,” according to Dr. Paul E. Phrampus, FACEP, FSSH, CPE, is defined as a combination of online educational materials and in-person learning, and this design can enhance the efficiency and effectiveness of simulation-based curriculum. Pre-work can be created de novo or it can be assigned from another source, if appropriate. By preparing for in-person simulation with pre-work, learners can be more prepared for and can engage in the simulation with a higher level of knowledge and critical thinking. When learners approach a simulation with a foundation of the material, didactic or procedural, knowledge can be applied rather than solely absorbed. Hybrid learning also benefits both the learners and educators as it enhances the potential complexity of the simulation.
Tips for Implementing Hybrid Sim From Dr. Phrampus
· Start with a needs assessment to guide expectations and outcome measures.
· Begin with the end in mind by creating a detailed list of exactly what learners should know or perform prior to generating or gathering learning materials.
· Incorporate active learning in the pre-course material.
· Ensure learners are clear on their responsibilities associated with the completion of the online materials and what the consequences are if they do not.
· Link the pre-work to the simulation to create an integrated continuum of learning.
What are the implications of this as it relates to emergency medicine training? I think it helps to understand adult learning principles to optimize how we learn, particularly given the time constraints on- and off-shift for education and studying, the nature of many emergency medicine procedures as “high stakes, low frequency,” and the growing emphasis on patient safety in healthcare.
There are so many educational resources and methods by which residents can acquire and practice emergency medicine: journals, question banks, foundations/role play, blogs, podcasts, procedure videos, virtual reality, task trainers, high-fidelity manikins, standardized patients, etc. Given the principles above and the aforementioned limitations on resident learning, I think it is wise to assess and frequently re-assess how best you learn. Further, if curriculum is not meeting your needs, how can you adjust the material or the method by which it is delivered? In addition, when you are instructing learners such as medical students or junior residents, think of these principles as you are delivering education and adjust according to your learner.
ABOUT THE AUTHOR
Dr. Nicole Rettig is the Director of Simulation at the University of South Florida Emergency Medicine Residency Program.