Kirk's Story - A Personal Reflection of Faith, Perseverance, and Triumph
My youngest son Kirk was born on a cold, January morning at Geisinger Medical Center.
My strong, resilient wife had been on bedrest for the previous 9 weeks for placenta previa. Her bleeding suddenly worsened, so we jumped in the car while our neighbors came over and took care of our other three children, Jake (6), Lindsey (4) and Whitney (2).
The C-section was as uneventful as an emergency C-section can be. Kirk's Apgar’s were 7 and 9, better than his older brother Jake's of 4 and 9. Things appeared OK for the first few minutes, then a sudden sense of urgency appeared on the incubator side of the operating room. Suction, nasal oxygen followed briskly by mask, then Kirk was quickly whisked out to the neonatal intensive care unit.
We had been blessed with a terrific Geisinger pediatrician, Dr. David Turkewitz, who had done an outstanding job taking care of our other three children. Uncharacteristic of David, he was nervous as he explained to us what was going on.
Kirk was intubated in the NICU followed by bedside echocardiogram. His brother Jake had surgery at Boston Children's Hospital six years prior for complex congenital heart disease (ASD, VSD, PDA, pulmonary vascular sling), so suspicion was high for something similar. Aorto-pulmonary window was seen on the bedside echo along with the diagnosis of persistent fetal circulation, prompting phone calls to quaternary pediatric centers in the region.
Dr. William Norwood (founder of the Norwood procedure) was then practicing at Children's Hospital of Philadelphia (CHOP). Unfortunately, Dr. Norwood was out of the country at the time. The Geisinger pediatric subspecialists reached out to Boston Children's Hospital for transfer to the care of Dr. Aldo Castenada, who had operated on Jake in 1983. The superb neonatal team of Geisinger Life Flight then transported my intubated 9-hour old son 360 miles to Boston Children's while I drove to the local airport to catch a commercial flight to Boston.
It was around midnight when I finally reached the pediatric cardiology intensive care unit at Boston Children's Hospital. I was met by a very bright but grim-looking pediatric cardiology fellow who cut right to the chase:
He said he did not expect Kirk to survive the night, and that I should get his mother to the hospital as soon as possible. I told him that was not possible as she was still in the hospital in Pennsylvania recovering from a C-section.
We needed a better plan.
I will never forget when the fellow handed me Kirk's arterial blood gases on a small piece of paper (as best as I can remember), pH-7.02, PCO2-101, PO2 -37 on FIO2 of 100% with 10 of peep. He anticipated my next response and said, "No, the PCO2 and PO2 are not reversed, and were drawn directly from his arterial line."
The sudden, overwhelming realization of what was really going on finally hit as I tried in vain to hold back the tears.
The plan now was to bring down the neonatal fellows from their NICU and have them use their expertise with the ventilator. After the NICU fellows did their magic with the dials, their best efforts got us into the "60/60" club.
The 2 am decision now is for Kirk to go on ECMO.
Unfortunately, there were no open ECMO beds at Boston Children's, but they did find an open machine at Massachusetts General Hospital. Ground EMS was called, and an outstanding NICU team again transported Kirk, this time across town to Mass General.
A very kind nurse drove me in her Ford Fiesta from Boston Children's to MGH as she had just completed her shift at 3am.
Back to another pediatric ICU waiting room where I am told they are cutting down on Kirk's right carotid artery and internal jugular vein. Dr. Dan Doody (real name !!), the pediatric surgical fellow on call, with the patience of a saint and tremendous skill, calmly cannulates his tiny vessels and hooks up the large clear hoses to the humming ECMO machine. Arterial blood gases improved but Kirk was now unresponsive to voice or pain.
He remained unresponsive for the next five days.
I never prayed so hard in my life.
Visitation was 10 minutes every two hours. I would sit to his right, stare at these two seemingly giant tubes coming out of his neck, tracking behind his right ear and then down into the ECMO machine. Those 10 minutes flew by quickly, then I was shushed back to the waiting room with the other anxious parents.
Alone for hours, I bargained with God.
I begged Him to take me and let Kirk live.
Please, please dear God, take me, and let Kirk live.
I've already had my time. Take me please, and let him survive.
Then back to visit with Kirk.
I spoke to him endlessly. I told him about his mother, his older brother and two sisters. I sang all the nursery room songs and lullabies I could remember. The NICU nurses tried to reassure me that Kirk had been through so much during his first 24 hours. They said he wasn't moving because he was just very tired and needed to rest.
But for the next five days, he remained unresponsive.
I flicked his feet when the nurses weren't looking, but still Kirk did not move.
On Day 6, I spoke to him, touched his foot.
And then he moved. He freakin' moved !!!
Dear God, thank you!! And now he is finally responding. The power of faith and prayer.
And now what's the plan.
Dr. Doody took Kirk off ECMO, and repaired both his right carotid artery and internal jugular vein. The jugular vein eventually went down but the carotid is still patent today (confirmed by “self-ultrasound” - please note Dr. Charlotte Derr !!). His aorto-pulmonary window now needed repair.
So back to Boston Children's Hospital so Dr. Aldo Castenada can operate on him the following week. Almost six years prior to the day, Dr Castenada had operated on Kirk's older brother Jake at the same hospital. I am told there are no coincidences, only miracles we fail to recognize.
Kirk's mother Alison finally arrived from Pennsylvania on Day 7. Kirk had an unremarkable postoperative course from his A-P window repair. His chest tubes were pulled, he was extubated, and then flown back to Geisinger to complete his hospitalization.
At week 5 of Kirk’s hospitalization, his mother developed a pulmonary embolus and was also hospitalized. She recovers well with 3 months of coumadin after IV heparin.
Kirk eventually gets discharged home from Geisinger and introduced to the rest of the family.
His dyspnea still persisted despite his surgery, and Kirk is admitted for RSV at age three months.
Note to self, when you see two seasoned pediatric specialists look pale and nervous after a procedure, take notice. Dr. Bill Gibson (pediatric ENT) and Dr. Stephen Wolf (pediatric pulmonologist) took Kirk to the OR for bronchoscopy. Once they got passed the cords, his airway narrowed severely. All they could see was a tiny ~1-2mm opening that scared the crap out of both of them. They very slowly eased out their scope and promptly called Boston for help.
The doctors had found a severely narrowed segment of tracheal stenosis. The decision now is to stop the steroids and return to Massachusetts General for tracheal resection while on cardiac bypass.
So back to Mass General at age 5 months for tracheal stenosis surgery. In order to relieve the tension on the suture line, a full-body cast from head to hips with sheepskin straps was constructed to hold Kirk's neck in constant flexion for the next two weeks. It was a challenge to bathe and change his diapers, but his Mom, with the patience of Job, got us through yet another challenge.
Dr. Turkewitz and the pediatric cardiology team at Geisinger continued to follow us. Kirk’s persistent right pulmonary artery stenosis was monitored with frequent echocardiograms. His secondary VQ mismatch was also followed with serial nuclear medicine studies.
At age 5, pulmonary artery angioplasty was attempted, but the artery remained dilated only for a short period of time.
Kirk continued to thrive with soccer and golf but was more of a fisherman, like his maternal grandfather. At one time he even entertained becoming a professional bass fisherman. And of the four kids, of course he is the daredevil of the group, crashing golf carts on our farm and invariably skateboarding without shoes, shirt or helmet when we are not looking.
At age 17, he does a "superman" off his skateboard with pretty severe road rash and a deep laceration down to the anterior superior iliac spine. After scrubbing out the asphalt and suturing, Kirk finally takes it easy for the next two weeks. He sees his cardiologist for a routine echocardiogram, and for some unknown reason his ejection fraction is now down to 20%. Usual meds are started, but the ejection fraction does not improve. His new MUSC pediatric cardiologist calls me and talks about AICD and possible "heart transplant list"……. and my heart once again flies back into my throat.
More intense prayer.
More bargaining with God.
Through His grace and a healthy tincture of time, Kirk's ejection fraction does gradually improve.
But the nagging right pulmonary artery stenosis and the persistent VQ mismatch remains, so something has to be done. There is not a big demand for pulmonary artery stents in 22-year-olds, so MUSC cardiology has to improvise. There is a biliary stent that fits the bill. They place a biliary stent in his right pulmonary artery and put him on aspirin.
Kirk has steadily improved since the pulmonary artery stent placement at age 22 and at his last cardiology appointment his ejection fraction is up to 50%.
Husband to his beautiful wife Megan, surfer, fishing enthusiast, paddle-boarder, swimmer, dog owner of a big black Lab named Ozzy, and running the occasional 5K are just some of his usual activities.
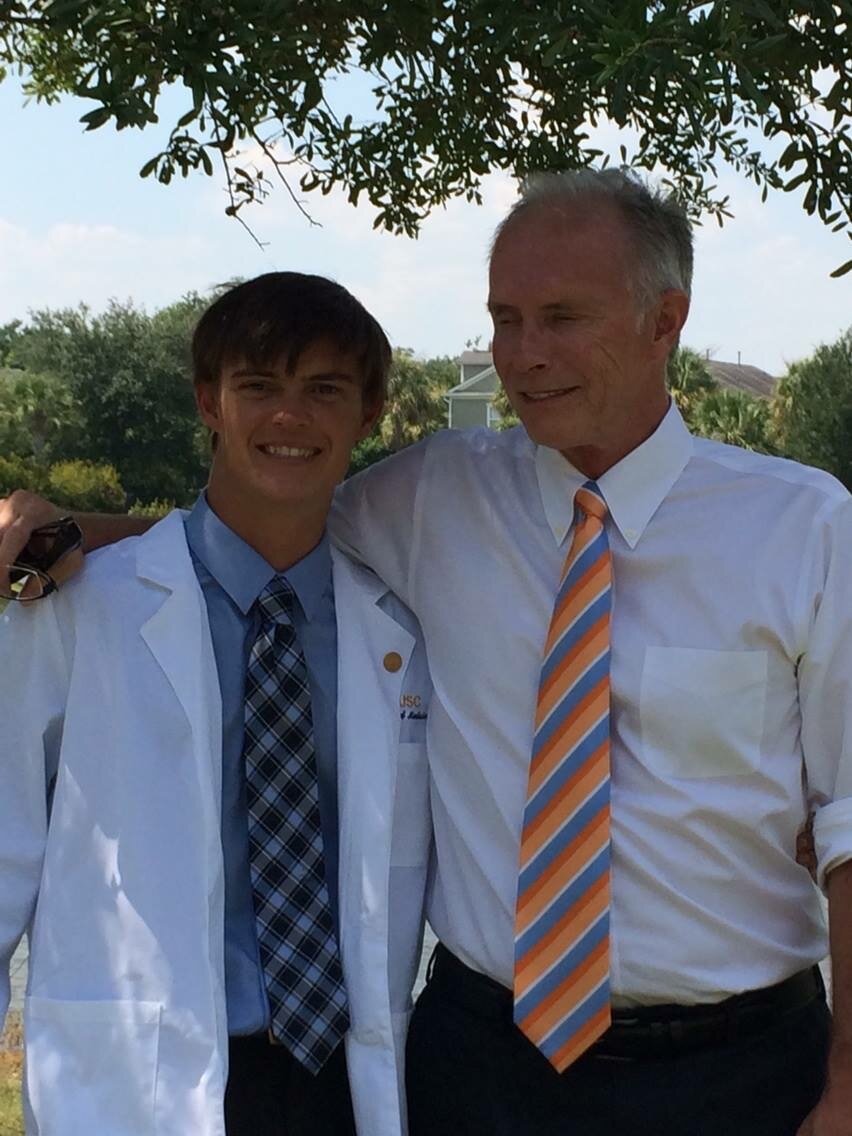
Oh, and by the way, Kirkpatrick James Gillen graduated from medical school at MUSC three years ago. I just reread that sentence and tears came to my eyes once again.
And I had the humble and distinguished honor of hooding Dr. Kirkpatrick James Gillen at the MUSC medical graduation in Charleston.
All of my prayers have been answered.
God had a plan.
Not my plan......something better.
Kirk started his surgical internship in July 2018 and is presently a second year radiology resident at MUSC with plans for fellowship in interventional radiology.
Kirk's siblings are all doing great as well.
His older sister Lindsey is the former student services coordinator for Clemson University, now a super-busy mother of three. His younger sister Whitney is a board certified optometrist in private practice in Greenville, SC. Older brother Jake graduated from his general surgery residency at U Va. and is now practicing as an acute care surgeon at Carilion Clinic in Roanoke.
I am beyond grateful for all of the tremendous physicians, nurses, EMS and support personnel that have helped my family over the years. Through God's enormous grace, all of my children are alive and well and thriving.
“We all go through difficult times in our lives, especially in emergency medicine. We are not defined by our challenges, but we are defined by how we handle them, and how we recover afterward. ”
Though not perfect by any means, prayer and a faith in a Higher power has blessed me beyond my wildest dreams.
I am truly grateful.
I can now look back and see the bargain I made with God many years ago came true.
And through His grace, mercy and wisdom, everyone survived.
- James P. Gillen MD
ABOUT THE AUTHOR
Dr. Gillen is Director of Emergency Medicine Education for USF and has served on the core faculty since 2008. Outside of work he is a proud father, dogfather, grandfather and the lucky husband of Marlene Gillen.